Cystectomy and Urinary Diversion
There are many reasons the bladder might need to be removed. These include cancer, bad infection, radiation damage, and neurologic damage to the bladder that is beyond repair. Most surgeons who remove the bladder focus on bladder cancer. Dr. Elliott is unique in that he focuses on bladder removal for non-cancer reasons. He has performed this operation over 200 times.
Steps of the operation: Cystectomy
Step 1: The abdomen is opened. While this can be done through an open incision or robotically, Dr. Elliott usually performs this through an open incision (in the lower half of the abdomen) because many of his patients have had multiple prior operations or radiation and he feels it is faster and safer through an open incision.
Step 2: Free the bladder from the side walls of the pelvis and other surrounding organs. This can be particularly difficult after radiation due to the amount of scarring that occurs.
Step 3: Divide the blood supply to the bladder. Again, this is more challenging after radiation.
Step 4: Divide the ureters which are the tubes that carry urine from the kidneys to the bladder.
Step 5: Separate the bladder from the rectum (in men) or vagina (in women) and remove the bladder. After prostate radiation the bladder can be especially stuck to the rectum. After cervical radiation the bladder can be especially stuck to the gynecologic organs. Occasionally, Dr. Elliott will leave a dime-size piece of the back wall of the bladder on the rectum or vagina in order to avoid injuring those structures.
Step 6: Proceed with Ileal Conduit Urinary Diversion or Indiana Pouch. Due to the amount of radiation damage to the bowels we usually perform ileal conduit in these patients. Patients who opt for an Indiana pouch must understand the responsibility to catheterize the pouch ever few hours. Additionally, in advanced age it will become more difficult to care for the pouch and an ileal conduit may become a better quality of life choice.

kidney
ureter
bladder
prostate

kidney
ureter
bladder
prostate
Ileal Conduit
An ileal conduit is a passive, low-maintenance, way to drain the urine from the body. We can’t connect the ureters directly to the skin to drain the urine because their blood supply won’t reach the front of the body. So we use the intestine as a bridge, or conduit, to carry the urine from the ureters (in the back of the abdomen) to the front. Urine drips from the conduit constantly and is caught by a bag that sticks to the abdominal skin around the stoma with an adhesive. There is a spigot, or valve, at the bottom of this bag that you turn in order to drain it. Most people replace the bag and the adhesive section every 3-5 days.
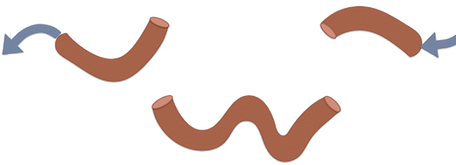
Step 1: Divide about 18-20cm (7-8 inches) of ileum (the last section of small intestine), keeping it attached to its blood supply but separating it from the flow of digestion (figs. 3-4).

food/stool going
toward rectum
segment for urinary diversion
food/stool coming from stomach
18 cm
Fig. 3: Intestine cut twice to isolate segment for Ileal conduit.
food/stool going
toward rectum
segment for urinary diversion
18 cm
food/stool coming from stomach
Fig. 4: Conduit segment separated from the rest of the intestine.
Step 2: After isolating the segment for the conduit, reconnect the bowel with stitches (fig. 5). Wash out the conduit segment.

food/stool going
toward rectum
segment for urinary diversion
18 cm
food/stool coming from stomach
Fig. 5: Intestine reconnection.
Step 3: Sew the ureters to the back end of the conduit (fig. 6).

kidney
ureter
Fig. 6: The ureters are sewn to the back end of the intestine. The front end is brought out through an opening on the abdominal wall, usually to the right of the belly button.
intestinal conduit
Step 4: Bring the front of the conduit up through an opening in the stomach muscle and the abdominal skin to form a stoma (fig. 7).

Fig. 7: The stoma is stitched to the skin on the abdominal wall.
Indiana Pouch
An Indiana Pouch is a way to store urine inside the body in a sphere-like pouch that acts like a new bladder in that it holds the urine until you empty it. This pouch is emptied by passing a catheter painlessly through a short tube of intestine (we call it a channel or stoma) from the belly button down into the pouch. This must be done about five to six times a day. The advantage of the pouch is that you don’t have to wear a bag; the disadvantages include a longer operation, a higher risk of urine infection and stones in the pouch. Also, you must be very disciplined about catheterizing the pouch on a regular schedule and flushing it out with water once a day.
Step 1: Divide the last 10cm of the small intestine (ileum) and the first 25cm of the large intestine (colon) from the rest of the bowel. It is very important that we use this particular segment of bowel because (as will be shown later) we rely on a natural valve between the ileum and the colon for the continence of the pouch. The colon will become the pouch and the ileum will become the channel.

small intestine
Fig. 8: Intestine cut twice to isolate segment for pouch.
Food/stool going from
colon toward rectum
colon/large intestine
Food/stool coming
from stomach through
small intestine
Step 2: Remove the pouch segment from the rest of the intestine and wash it out so there is no stool in the pouch.

Fig. 9: Intestine cut twice to isolate segment for pouch.
10cm
25cm
Step 3: Reconnect the small intestine (ileum) and large intestine (colon). We use a stapler for this.
Fig. 10: The two ends of the intestine are reconnected.

kidney
ureter
Food/stool coming
from stomach through
small intestine
Food/stool going from
colon toward rectum
intestinal conduit
Step 4: Open up the colon segment that will become the pouch. We do this by unzipping it along one wall. Fig. 11 illustrates the outside of the colon in dark brown and the inside (or mucosa as we call it) in pink.

folded down
Fig. 11: Intestine is washed out. The colon portion is opened lengthwise.
Fig. 12: Colon is opened wide. The inside of the colon is shown in pink. Small intestine is narrowed to the size of a catheter by cutting out some of its diameter and then sewing it closed.
Fig. 13: A natural valve between the small intestine and colon keeps urine from leaking out the stoma.
Step 5: The ileal segment is tapered (or narrowed) using a scissors and stitches, or using staples that cut and staple at the same time. The goal is to get the ileum narrowed until it is about the width of a catheter. The ileum is normally about as wide as a toilet paper tube; if you tried to catheterize through that, the catheter would get lost in the tube. Therefore, we narrow the newly constructed tube so that the catheter slides in a straight line. With the colon opened, you can also appreciate the valve between the ileum and the colon that will serve as the continence mechanism that keeps urine from dripping out of the ileal channel (and out your navel) when the pouch gets full. When properly functioning, only a catheter can open that valve. The colon is then folded over to begin to create a sphere (figs. 12 and 13).
Step 6: Continue the folding of the colon and sewing the edges together. Much like a baseball which is made out of two flat pieces of leather sewn together, we are able to make a sphere (or pouch) by folding and sewing the colon (fig. 14). The continence valve is shown as a ring where the ileal channel and colon pouch come together.

Fig. 14: The edges of the folded colon are sewn together, making a pouch. Stitches are added at the valve between the small intestine and colon in order to tighten the valve.
Step 8: The ureters are sewn to the pouch, and the end of the ileal channel is sewn to the abdominal wall, usually at the navel, but sometimes to the right of the navel.

Fig. 15: The ureters are sewn to the pouch and the stoma is send to the abdominal wall, usually at the belly button.
